
According to the urban dictionary, Left Turn can mean "an unexpected change in events." That would describe my day. It felt like a whirlwind.
Normally, Monday’s are operating room days. There are 6-10 major surgeries and many minor procedures scheduled. I went into our morning report with the medical students as usual, after which I headed down to maternity. It was more chaotic than usual, with 2 patients bleeding with placenta previa (placenta blocking the cervix), one woman with a miscarriage that was bleeding, and a grand multip (lots of kids already) with a normal labor but with the breech (bottom) coming first. I quickly made plans… let’s do a C section ASAP for the one at term, give medication to stop the labor for the second, and reevaluate the lady with the miscarriage. The grand multip could continue her labor without interference or medicine. When things were in a semblance of order, I headed over to the OR, both to inform them of the incoming C section and also to start our long list of procedures.
BUT----When I got near the door, I was met by a staff
doctor, informing me that all the doctors in the hospital were called to go to
a “nearby” village to vote in person for something. So surgeries were canceled
that day… all of them, and now I was supposed to go on a 2 hour drive over
bumpy rutted roads to cast a vote. I rushed back to the maternity where we
performed our first C section in the new maternity OR!! The novelty of it and
the celebration it really deserves were dampened a little by the stress of the
change of the day, and the need to get done quickly so as to get ready for a
trip. I'll celebrate it a bit with several pictures of opening day before continuing the story.
 |
| Chief of the operating room standing by the new maternity OR bed and lighting. |
 |
| Preparing the first case in the maternity OR-- a C section for placenta previa |
 |
| Praying together before we make the incision to start the surgery |

Sure enough, I was just scrubbing out as the assistant was closing the skin when I was told to finish quickly because the vehicle had been prepared and other doctors were waiting on me.
I started panicking just a bit. I hadn’t pumped or fed Zack
since 6:15am and it was already after 11am. I had to go back to the house. I
was going to miss lunch. I had no idea when I’d get back- afternoon or evening.
I finally decided the prudent thing to do would be to simply take Zack with me,
endure the 2 hour roads there and back, but at least not be out of control with
his needs. I ran back, Ryan helped me gather water, diapers, changes of clothes
for Zack, and I stuck in a jar of peanut butter. That’ll do in a pinch. My
phone rang but I missed the call. I was out of units to call back. I was certain
they were calling to say they were about to leave. And I started off down
towards the waiting vehicle. A woman called after me on the path, waving her medical
chart paper. I felt completely overwhelmed by everything going on, by the still-bleeding
patients in the maternity, by the need to take care of my son, by the heat of
the midday sun beating on us, by the total and utter randomness of the change,
and by my incomprehension as to what we were doing this for.
BUT----When I arrived at the vehicle, it was neither ready,
nor filled with waiting doctors. It really was quite confusing. Zack was
stirring in the baby carrier, wanting to be fed. It was hot. Two of the
doctors, seeing me with Zack and a little harried from rushing around all
morning, suggested that it wasn’t so important that I go. I had a hard time
understanding what was so important that all the doctors of the hospital were
told they should go and thus the operating room schedule had been canceled so
abruptly, if indeed it weren’t so important that I go. But in the end, I started
back up to the house, a little sheepishly as I was still uncertain of the
decision. I called a couple other doctors to try to understand this situation more culturally, but in the end I
decided to stay.
I readjusted my expectations to be the bleeding ladies who needed treatment in the maternity. Sure enough, I got a phone call that the second patient with placenta previa needed a c section because her hemoglobin had dropped from 8.7 to 4.5. Even though the baby would not make it, and just by a few weeks, we needed to save the life of the mother*. I hurried to feed Zack, and ran down to do the C section.
BUT----She
was still in the maternity, lying just as she had when I had left her. Though the
C section didn’t seem quite as urgent as I thought initially based on the phone
call, I did agree with its necessity. She wasn’t gushing blood, but with a very
low hemoglobin, starting a C section before finding a blood donor didn’t outweigh
the risk. It’s the family/assistant of the patient that has to find someone to
donate blood or pays $10 for the lab to find a donor in the community to keep
the blood in the bank. This can take time, sometimes hours. So I trudged back
up the hill to catch the end of lunch with the family. By now, it was almost
comical to see Ryan’s face when I walked in the door not having done what I had
expected to do moments before.
The rest of
the day was pretty straightforward without further huge left turns. I nearly
cried with the baby who we delivered just a few too many weeks early to survive
here. It would likely have done well in the US. It did cry, and was sent to
pediatrics for as much support as we can give here, but if it survives the
night, I’ll be surprised.** I then headed over to see about doing a dilation
and curettage for our bleeding miscarriage. However, she met me on the sidewalk
and said she felt like she had passed something since the ultrasound that
morning (which had showed retained products of conception) but lamented the
fact that the placenta always stayed in. Unfortunately, she had already had 4
miscarriages. I decided she needed further evaluation again before taking her
to the operating room.
It was
amazing! As in, I’ve never seen it except in cool professional photography. The
gestational sac with the 10 week old fetus had come out intact with the
medication we had given. We were able to see the fetus floating in the amniotic
fluid, with its formed arms and legs, spinal cord, and head. Its heart had
stopped beating long ago, but it was amazing to see this tiny being just a bit
bigger than a gummy bear. So cool!!
The emotional sting of the miscarriage had dulled
over the two days since its diagnosis, and the mother was truly fascinated by
the tiny being that had been growing inside her. She and her husband both
wanted to see it, which is very rare in this culture. Afterwards, I used an
ultrasound (from our new mobile ultrasound available in the maternity!!) to
check to see if she had anything left in the uterus requiring further
management. Fortunately for her, she did not need it. I asked her for
permission and then proceeded to teach about 15 medical students, nursing
students, and nurses the basics of ultrasound as we looked at her uterus, her
bladder, her liver, her abdominal aorta, her kidneys, and her heart. It’s a joy
to be able to see the wonder of learning something for the first time.
 |
| 8-10 wk fetus inside its intact amniotic sac |
 |
| The new ultrasound is mobile, so we can easily move it into the delivery room if we have an urgent need for further evaluation. |
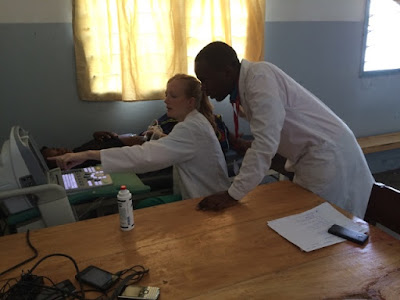 |
| Teaching ultrasound in the new maternity ultrasound and consultation room |
As I headed home in the evening, I was greeted on the path by my kids with Nancy, their beloved nounou (nanny in French), who will be leaving at the end of the week. She graduated from high school and won’t be living here any longer except for limited periods. This season of life is coming to an end for Sydney- Nancy has been with her sporadically since the very evening of her birth and daily since she was 9 months old. We are all happy for Nancy, but very sad to see her go. At any rate, I joined them as they walked down to the Rices’ house. We had pineapple ice cubes for a snack, went and jumped and played in the river with Tim and Ryan also joining us. We ate dinner at the Rices’ and afterward came up to our house, put the kids to bed, and watched the second half of a movie we’d started. Overall, despite the crazy changes in expectation, it was a great day!
*From the Dublin Declaration 2012, an international consensus
regarding abortion to save the life of a mother. “As
experienced practitioners and researchers in obstetrics and gynaecology, we
affirm that direct abortion – the purposeful destruction of the unborn child –
is not medically necessary to save the life of a woman. We uphold that there is
a fundamental difference between abortion, and necessary medical treatments
that are carried out to save the life of the mother, even if such treatment
results in the loss of life of her unborn child. We confirm that the
prohibition of abortion does not affect, in any way, the availability of
optimal care to pregnant women.”
**The baby has, in fact, defied all odds and is still alive. As a colleague of mine said as we encouraged the nurses to make the normal efforts in neonatal resuscitation at the C section, "We think the baby is too premature to live, but God can still do a miracle."








